News
11 April 2025
Road to Research: Q&A with Alex Garruss, Ph.D., Jim and Virginia Stowers Fellow
“There are few rewards as powerful and as elevating as making a clear, robust scientific observation that advances the field.”
Read Article
News
Stowers team develops novel assay to identify genes controlling pharynx regeneration in flatworms
KANSAS CITY, MO—As multicellular creatures go, planaria worms are hardly glamorous. To say they appear rudimentary is more like it. These tiny aquatic flatworms that troll ponds and standing water resemble brown tubes equipped with just the basics: a pair of beady light-sensing “eyespots” on their head and a feeding tube called the pharynx (which doubles as the excretory tract) that protrudes from a belly sac to suck up food. It’s hard to feel kinship with them.
But admiration is another thing, because many planaria species regenerate in wondrous ways—namely, when quartered they reconstruct themselves from the pieces. Sliced through the “waist”, they regenerate the missing tail or head; bisected lengthwise, worms duplicate their mirror image. This capacity is not what’s surprising, as biologists know that 30% of their body cells are stem cells. The question is, how do stem cells in a planaria fragment know how to generate what’s missing?
In the April 15, 2014 issue of the online journal eLife, Stowers Institute for Medical Research Investigator Alejandro Sánchez Alvarado and colleagues address that issue by identifying genes worms use to rebuild an amputated pharynx. They report that near the top of the pharynx regeneration hierarchy is a master regulator called FoxA. These findings support an evolutionarily conserved role for FoxA proteins in driving construction of endoderm-derived organs and reveal how stem cells sense loss of a particular structure on a molecular level.
Mammals can deploy adult stem cells to replace skin or immune system cells, among others. But when it comes to re-creating entire structures, amphibian, fish and planarian species are the champs. “When mammals are severely injured, they just heal the wound and call it a day,” says Sánchez Alvarado, who is also a Howard Hughes Medical Institute Investigator. “But if a salamander loses a limb, it will first heal the wound and then start assembling the missing parts. Right now, the mechanisms cells use to realize what structure is missing and then restore it remain completely mysterious.”
To unravel the mystery, the team conducted two “screens”. First, they amputated the worm pharynx, which prohibits feeding for about a week as planaria rebuild a new one. Around day 3 post-amputation, the team conducted microarray analysis to identify any gene switched on by amputation and amassed about 350 candidates. To test them, they then fed inhibitory RNAs designed to suppress expression of each gene separately to new batches of worms, repeated the amputations and observed whether worms regained feeding ability. That narrowed the list to 20 candidates that when lost hampered feeding and in most cases interfered with pharynx formation.
According to Carrie Adler, Ph.D., a postdoctoral fellow in the Sánchez Alvarado lab who led the study, analysis showed most of the 20 factors either had a generic function in stem cells (which was interesting but not what they were after) or were specifically required for pharynx regeneration. Among the latter, one factor showing a particularly robust effect was a DNA-binding protein called FoxA. “Targeting FoxA completely blocked pharynx regeneration but had no effect on the regeneration of other organs,” says Adler.
High resolution microscopy analysis showed that stem cells ramped up FoxA expression soon after they converged on the amputation site. “Currently, we think that FoxA triggers a cascade of gene expression that drives stem cells to produce all of the different cells of the pharynx, including muscle, neurons, and epithelial cells,” says Adler. “The next question is how FoxA gets stimulated in the first place in only some stem cells.”
Researchers knew previously that during embryogenesis FoxA initiates formation of endoderm-derived organs in species as diverse as mouse and roundworms. The new work suggests that regenerating tissues exploit those evolutionarily ancient gene expression pathways. “Engulfing food is one thing that defines an animal,” says Sánchez Alvarado. “This means that organisms from humans to flatworms use a common toolbox to build a digestive system, one that has been shared since animals became multicellular.”
A fortuitous (in hindsight) setback facilitated the work. As a graduate student studying the roundworm C. elegans, Adler decided to test effects of roundworm anesthetics on flatworms. One, a sodium azide bath, put planaria to sleep but made their pharynxes drop off. Aghast, Adler soon realized that the azide solution (which planaria survived) left a uniform, minimally-destructive lesion. Thus was born the “selective chemical amputation method”, allowing large-scale analysis and reliable quantification of results and freeing researchers from tedious hours at a dissecting microscope.
But why go to such trouble to pioneer regeneration research in small animal models? The answer is obvious to both Adler and Sánchez Alvarado. “Because regeneration is limited and difficult to study in humans and mice,” Adler says. “Planaria have infinite capacity to regrow all organs. By understanding this enhanced ability we may learn how to accelerate mammalian regeneration.”
Sánchez Alvarado concludes that the work cements planaria’s place as a tractable model system to analyze regeneration or stem cell activity. “Planaria’s simplicity is what makes it such a fruitful system to answer questions relevant to regeneration,” he says. “If we used salamanders for these studies it would take 90 days to do an experiment. I want answers to these questions yesterday, not years from now.”
Also contributing to the all-Stowers study were Genomics Scientist Chris Seidel, Ph.D., and Sean McKinney, Ph.D., of the Microscopy Center.
The Stowers Institute for Medical Research, the National Institutes of Health, and the Howard Hughes Medical Institute funded the study.
About the Stowers Institute for Medical Research
The Stowers Institute for Medical Research is a non-profit, basic biomedical research organization dedicated to improving human health by studying the fundamental processes of life. Jim Stowers, founder of American Century Investments, and his wife, Virginia, opened the Institute in 2000. Since then, the Institute has spent over 900 million dollars in pursuit of its mission.
Currently, the Institute is home to nearly 550 researchers and support personnel; over 20 independent research programs; and more than a dozen technology-development and core facilities.
News
11 April 2025
“There are few rewards as powerful and as elevating as making a clear, robust scientific observation that advances the field.”
Read Article
News
09 April 2025
New study shows how we can better learn our genome’s hidden grammar, potentially paving the way for personalized medicine.
Read Article
News
09 April 2025
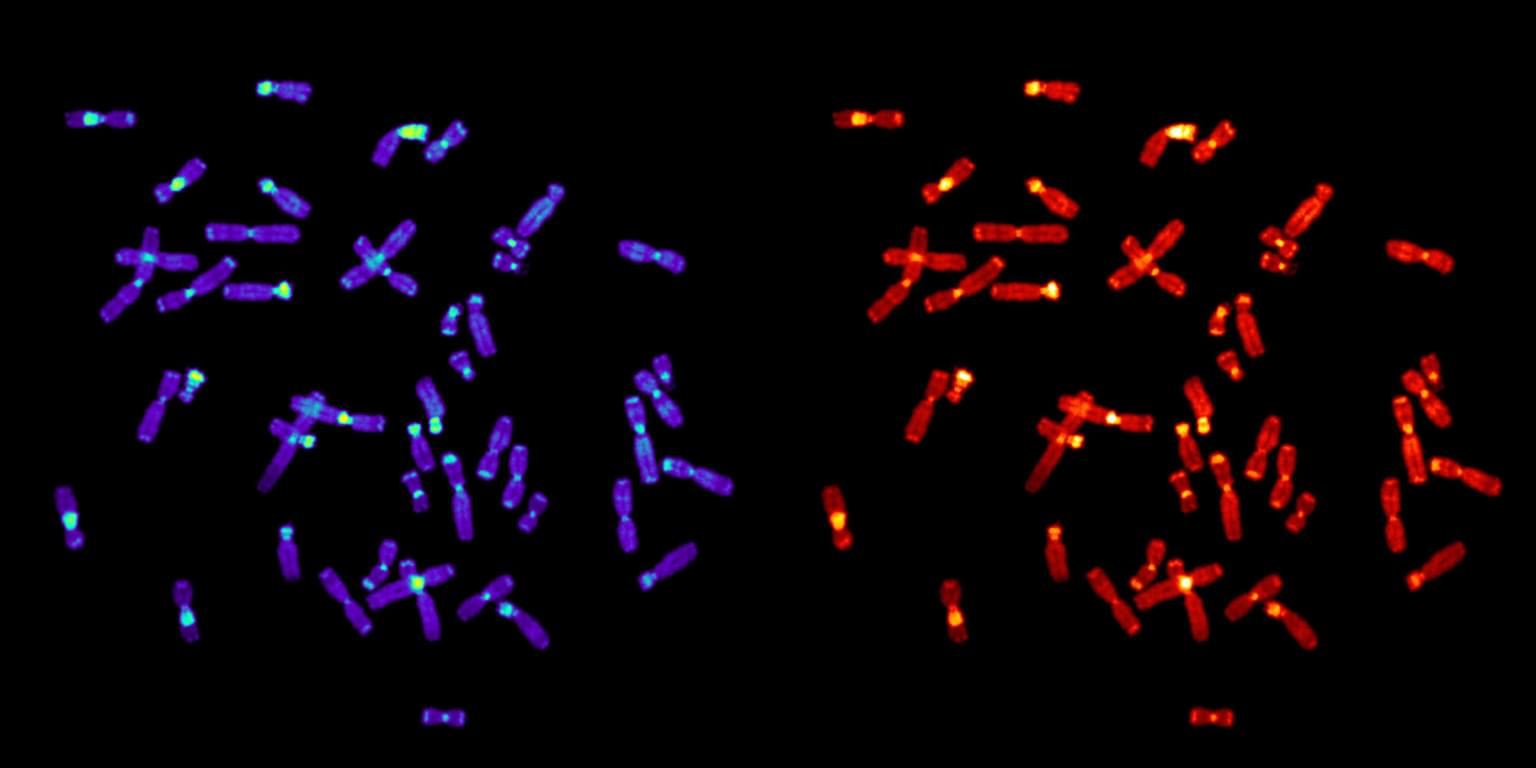
The multi-institutional study assembling six ape genomes provides a new appreciation for how chromosomes evolve.
Read Article
