News
11 April 2025
Road to Research: Q&A with Alex Garruss, Ph.D., Jim and Virginia Stowers Fellow
“There are few rewards as powerful and as elevating as making a clear, robust scientific observation that advances the field.”
Read Article
News
Discovery offers potential therapeutic target for certain cancers
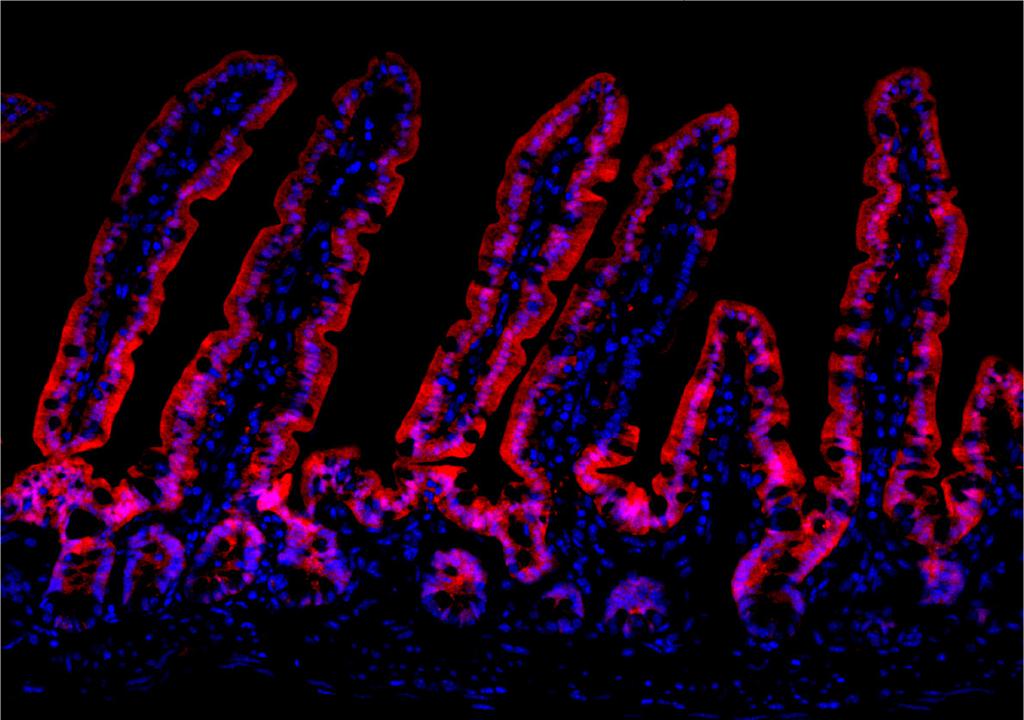
Fluorescent microscopy image showing Frizzled5 expression (magenta) within folds of mouse gut lining.
By Rachel Scanza, Ph.D.
Cells lining the gut must continuously replenish themselves for life-sustaining functions, making the gut one of the body’s most regenerative tissues. A healthy gut’s role includes digestion and nutrient uptake from food, the elimination of waste, and protection against harmful bacteria. However, the gut’s ability to regenerate new cells must be carefully controlled to keep unchecked cell division, a hallmark of cancer, at bay.
New research from the Stowers Institute for Medical Research has uncovered a protein that ensures the gut lining regenerates, specifically the layer of cells called the “intestinal epithelium” that forms the barrier between the body and the contents of the intestines. This key protein could provide a novel therapeutic target for treating intestinal and colon cancers.
“Humans renew all the cells lining the intestines each week,” said Stowers Investigator Linheng Li, Ph.D. “This constant renewal repairs damage and maintains the integrity of the gut barrier, which is essential for health.”
The study published in Developmental Cell on November 22, 2024, investigated the role of Frizzled5, one member of a protein family vital for tissue maintenance, in mouse intestinal epithelium. Led by Postdoctoral Research Associate Lu Deng, Ph.D., in the Li Lab with collaborators in Stowers Technology Centers, the findings uncovered that Frizzled5 is essential for intestinal stem cells to both self-renew and regenerate the epithelium. Disrupting Frizzled5 in specific epithelial regions revealed two distinct stem cell populations capable of replenishing each other.
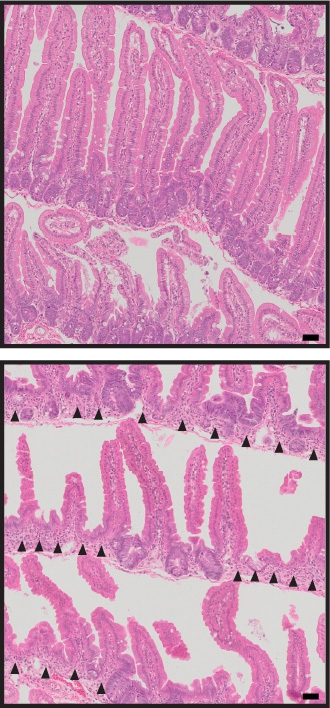
Cross section of gut lining in control mouse (top) and at seven days after silencing Frizzled5 in all intestinal epithelial cells where black arrows indicate crypt loss (bottom). Scale bar is 20 micron.
The intestinal epithelium is designed to maximize its surface area to allow cells to secrete and absorb nutrients and other molecules, with many folds forming finger-like protrusions. The base of the folds called crypts contain small numbers of actively dividing stem cells. These stem cells both self-renew and generate cells that move up the columns toward the fingers as they acquire specialized functions.
Questions surrounding where intestinal stem cells are located and how they can both replenish specialized cells for routine maintenance of the gut and repopulate themselves when damaged have remained largely unanswered. However, many individuals can recover from infections that severely damage the intestinal epithelium, suggesting built-in defense strategies to restore stem cells.
“Think of the intestine as having two resources of stem cells: fast-cycling cells for daily regeneration and slower-cycling ‘reserve’ cells that can be activated under stress,” said Li. “This ‘buddy system’ makes the gut robust.”
To identify how stem cells in the crypt are regulated, the team first examined many proteins involved in signals that play a crucial role in controlling cell division. A particular signaling pathway called Wnt is active during development and adult tissue maintenance but frequently disrupted in cancer. The researchers detected a known protein that binds Wnt signals in all intestinal epithelial cells—Frizzled5.
To verify that Frizzled5 plays a pivotal role in regulating intestinal cells, the researchers used genetically altered mice in which Frizzled5 activity can be impaired either in all intestinal epithelial cells or only in specific cell types.
“If Frizzled5 is lost from all intestinal cells, the crypts are destroyed,” said Deng. “However, silencing Frizzled5 in the fast-cycling crypt base cells allowed the cells higher up the crypt to replenish them, and vice versa.”

Graphical abstract of intestinal crypt model: Top left, normal crypt maintenance shows fast-cycling stem cells (green) at the base self-renewing and differentiating to generate specialized cells, with slow-cycling cells (blue) higher up replenishing base cells. Top right and bottom left illustrate crypt preservation when Frizzled5 is disrupted in either cell group. Bottom right shows loss of crypt integrity when Frizzled5 is disrupted in all epithelial cells.
The team then explored how Frizzled5 operates. Densely packaged DNA called chromatin needs to be unwound or “opened” to allow genes in that region to become active. Previous studies have shown that chromatin reorganization is required for intestinal cells to regain stem-like states. By combining two techniques to measure gene activity and chromatin accessibility, they found that Frizzled5 controls when DNA was open or closed, in turn driving cells toward stem or specialized types.
“On the cellular level, the gut has flexibility for renewal because there are two distinct stem cell reserves,” said Li. “On the molecular level, the mechanism our study has shown is that when Frizzled5 receives the Wnt signal, cell division and stem cell renewal are active. Lu found that Frizzled5 is required for reprogramming intestinal cells toward ‘stemness’.”
Many cancers arise by hijacking a cell’s stem cell capabilities for unlimited proliferation. Identifying a single protein with global control over cell fate makes Frizzled5 a novel target for treating cancers.
“Designing synthetic Frizzled5 agonists or antagonists—small molecules that increase or decrease Wnt signaling—may have therapeutic potential,” said Deng. “In cancer, Wnt signaling is typically amplified, so a drug that dampens Frizzled5 may help treat tumors.”
The Li Lab plans to continue examining how intestinal stem cells are regulated. “How and where stem cells in the intestines function has been debated for 15 years,” said Li. “Lu’s work along with other recent studies could change the direction of how we approach intestinal regeneration research.”
Additional authors include Xi He, Ph.D., Shiyuan Chen, Ning Zhang, Ph.D., Fengyan Deng, Ph.D., Allison Scott, Yanfeng He, Ph.D., Dai Tsuchiya, Ph.D., Sarah Smith, Ph.D., Michael Epp, Seth Malloy, Fang Liu, Mark Hembree, Qinghui Mu, Ph.D., Jeffrey Haug, Ermanno Malagola, Ph.D., Huzaifa Hassan, Kaitlyn Petentler, Rhonda Egidy, Lucinda Maddera, Jonathon Russell, Yan Wang, Ph.D., Hua Li, Ph.D., Chongbei Zhao, M.D., Ph.D., Anoja Perera, Timothy Wang, M.D., and Calvin Kuo, M.D., Ph.D.
The work was funded by NCI Cancer Center Support Grant (award: P30CA168524), the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (NIH) (awards: U01DK085507, R01DK11572802), and with institutional support from the Stowers Institute for Medical Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
News
11 April 2025
“There are few rewards as powerful and as elevating as making a clear, robust scientific observation that advances the field.”
Read Article
News
09 April 2025
New study shows how we can better learn our genome’s hidden grammar, potentially paving the way for personalized medicine.
Read Article
News
09 April 2025
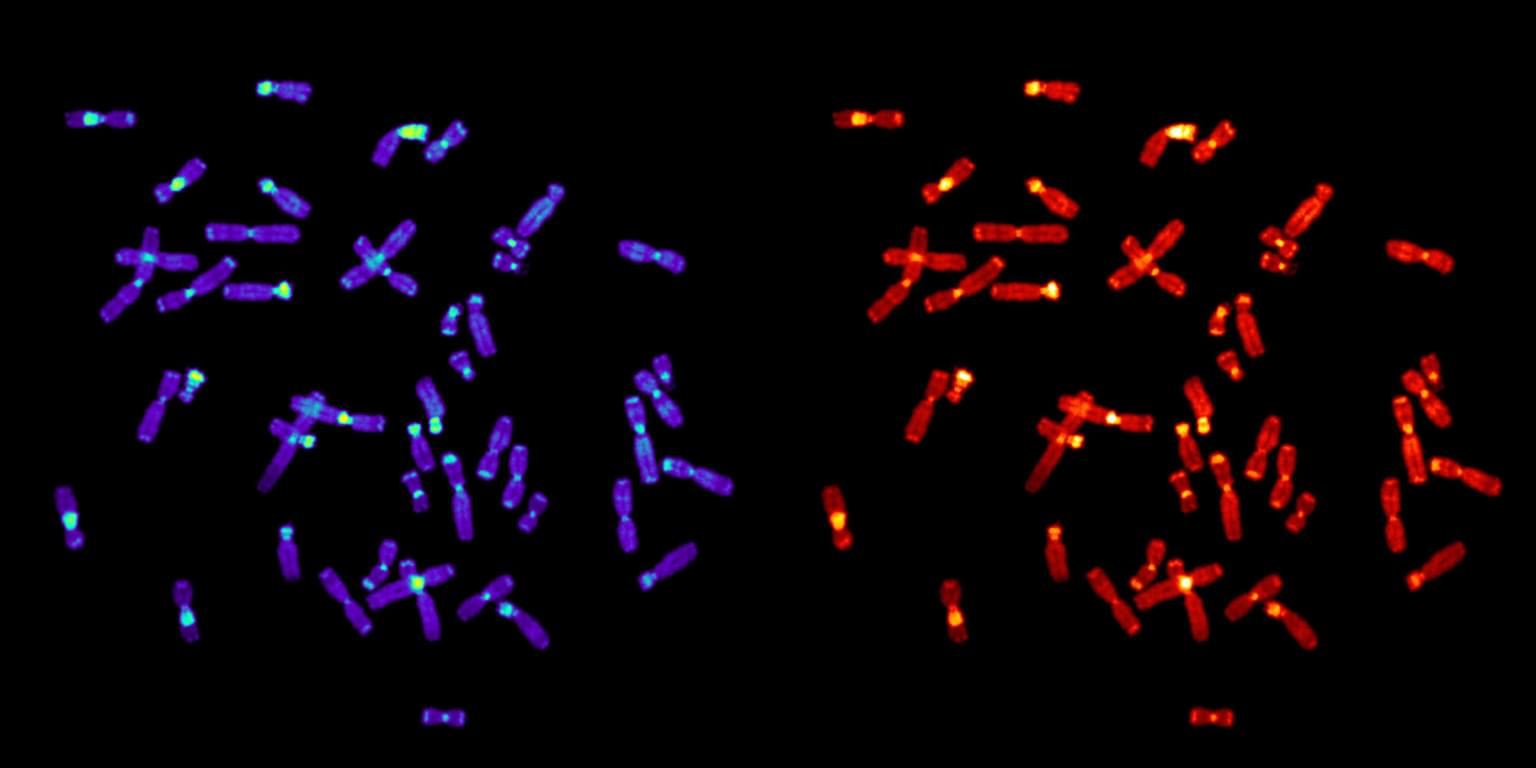
The multi-institutional study assembling six ape genomes provides a new appreciation for how chromosomes evolve.
Read Article
